Shin Splints: What are they and how do they occur?
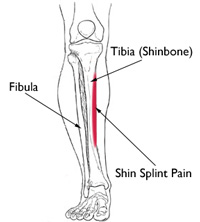
Shin Splints or “Medial tibial stress syndrome”, is a common term used among people to describe a pain in the leg in and around the area of their shin bone.
True shin splints occur when you experience pain on the inside of your shin bone, generally just a few inches above your inside ankle bone. The incidence rate varies from 4% to 35% in military and athletic populations (Batt ME & Batt M, 2011). Chronic presentations are more likely in females; those with a running history of less than 5 years; those with an increased body mass index; those with an increased hip rotation; people with standing foot pronation and a those with a history of orthotics use (Batt ME & Batt M, 2011).
Shin splints can happen on both shins or just on one, and they are normally due to a load issue. High load activities for the lower limbs include running, jumping/landing and agility work. The load or force reaches a point where the body cannot cope with excessive tissue breakdown and this results in pain. This injury can also be related to changes in the training program, such as an increase in distance, intensity and duration (Galbraith RM & Lavalee ME, 2009) or reduced recovery after these high load activities.
Assessing Shin Pain
At Dublin Sports Clinic, this issue would be assessed by examining the full history of the injury, related injuries and exercise history of the client. Then an assessment of their whole lower limb during basic movement patterns, single leg control and landing and running mechanics would be performed. The structure and surrounding structures of the shin bone are then looked at in a relaxed position.
Chronic symptoms of shin splints affect performance and could potentially lead to stress fractures. Therefore, symptoms should not be ignored if they continue to persist.
Treating Shin Pain
Treating this injury varies from person to person, but generally, the following steps are commonly used.
1) Get the patient exercising pain free
• Reduce the load –
Depending on symptoms, training will need to be modified for a duration of time. Treatment consists of reducing the training load to a level that does not flare up the shins.
• Offload the shin –
Release the tissue around the inside of the shin, lower calf and arch to reduce some of the pressure on the area.
Get muscles surrounding the arch, ankle and hip to kick in and help support their buddy!
Shock absorbing insoles or more formal orthotics may help to get the individual to a higher load before pain or stress is felt. Especially is there is a high rate of collapse around the arch when fatigue starts to set in.
2) Help the patient develop more awareness
• Learn what is happening around the shin to cause the stress. Feel what you need to do in static and low level dynamic positions to reduce the amount of stress on your shin. Start simple and push to more specific single leg work related to running patterns when possible. Developing control around the foot and hip to prevent as much stress going through the stabilizing structures on the inside of your shin is a key step.
3) Increasing strength and control
• Pure strength and higher level dynamic awareness –
Develop single leg strength and movement patterns using the whole chain of the foot, calf and hip. It is individual for each athlete but if it is not just a once off training error, a weakness is generally seen somewhere along the lower limb chain. If these muscles start to fatigue, stride patterns can alter. Strain can then develop and increase on the structures surrounding the foot and ankle.
4) Progress the load
• Strength/control exercises –
Use these exercises as rehabilitation, adding weight, repetitions and landing forces. Weight and repetitions speak for themselves and should be carefully progressed.
Training to improve shock absorption and spring as the foot hits the ground are added in once these activities can be done pain free. This impact work should be done in a non-fatigued state with the aim of improving bone load and work of the calf, ankle, foot and hip as you come in contact with the ground.
• Endurance/recovery –
Non-impact lower limb control work can also be done a slightly fatigued state, for example working upper parts on the chain like hip control while the feet are fatigued can help stimulate loading characteristics of longer runs without the effects of landing shock forces on the feet.
Recovery between training sessions need to be monitored closely.
Running endurance should be gradually built back up and progressed at a rate that the body and shins can tolerate.
Unfortunately, there is no one size fits all recipe for treating shin splints. Assessing and treating all the potential origins of the problem and understanding the common pitfalls with this injury is the key to full recovery from shin splints.
If you think you may be suffering from shin splints or a similar injury, contact Dublin Sports Clinic on 01-5517343 or [email protected] to book a physiotherapy consultation.
Blog by Catherine Simpson MSc. MISCP, Chartered Physiotherapist at Dublin Sports Clinic.
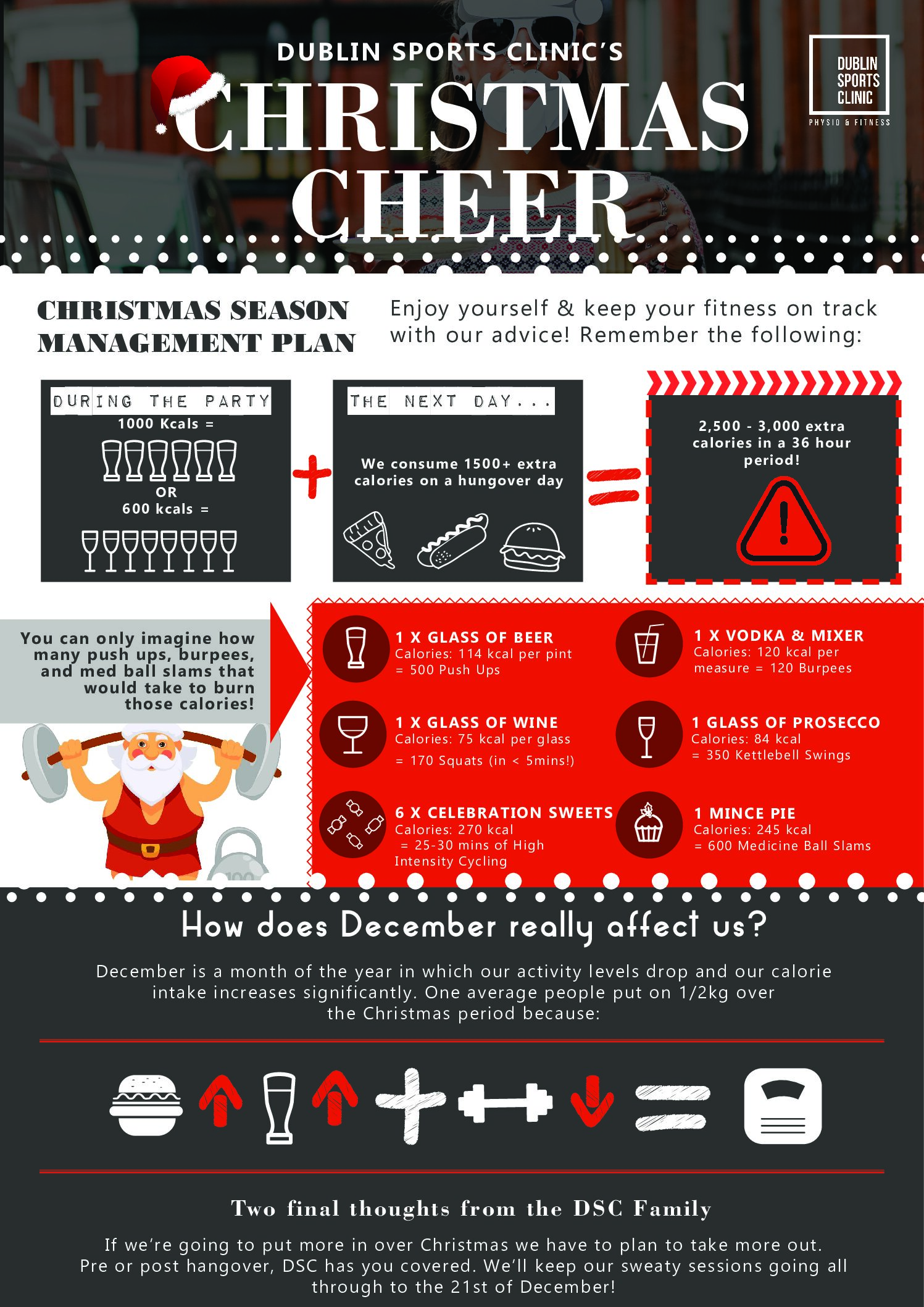
Staying on Track in December
Around Christmas time we have more work dinners, catch up with old friends, friends come home for the holidays and there’s a more family gatherings.

Member of the Month
Stephanie has been one of the most consistent and motivated clients I have ever trained. After ankle surgery a few years ago, our training journey

Top 10 Q’s October
How often should I train in a week? Easy – at least 4 times a week to achieve a healthy lifestyle. Your weekly exercise routine

